White House Rural Playbook
A guide providing communities with information on applying for a portion of the $1.2 trillion in funding now available through the Bipartisan Infrastructure Law.
A collection of resources curated for organizations interested in creating cross-sector health partnerships and increasing community investment in rural areas and small towns to create the conditions that support improved community health
A Playbook for New Rural Healthcare Partnership Models of Investments is an action-oriented guide designed for healthcare organizations who want to pursue partnerships with local community and economic development and other sectors in rural areas and small towns to create the community conditions that support improved community health. After interviewing dozens of experts we share case studies highlighting core strategies used by rural healthcare entities as examples for future multi-sector partnerships to follow.
This update demonstrates that multisector partnerships are the best way to improve health and prosperity in rural communities. This follow-up initiative is not just about collecting stories; it's about generating knowledge that can be shared and applied across the rural landscape. By amplifying the voices of those on the front lines, we can foster a community of practice that learns from each other's successes and challenges.
This project based in the Bemidji region of Minnesota described a community-wide effort in which the Sanford Health system stepped up to meet the needs identified by a Northern Minnesota Veterans Home Task Force by donating land for a new Veterans Home.

As of late January 2024, the Bemidji Veterans Home welcomed its first four residents . The new home is 80,000 sq ft and offers 72 units with a waiting list of over 300 veterans, clearly indicating the demand for this type of housing in the region. Sanford recently donated six acres of land to spark the development of new affordable workforce housing, a great need in rural communities across Minnesota.
As outlined in the original playbook, the launch of this project benefitted from a land donation by Sanford Health. The story of a health system donating land is having a broader impact as other health systems see opportunities to address social determinants of health through affordable housing.
Essentia Health, another integrated health system serving patients in Minnesota, Wisconsin, and North Dakota, donated land for the Brae View development, a 72 unit mixed-use housing development with much needed ground level childcare (110 slots) for both Essentia employees and community residents in the Central Hillside neighborhood of Duluth, Minnesota. Essentia has grown its community and impact investment work related to affordable housing using grants, a low-cost loan, and the donation of land. In partnership with the local YMCA, Essentia is contributing close to $3 million to the childcare portion of the project. Nearby are Brewery Creek Apartments (52 units) and Brewery Creek Terrace (21 units) side by side developments, one new and one rehab of a blighted property, that will bring new life to part of the community that has been neglected for decades. In total the 145 units of housing that are currently being developed are just steps from the hospital with potential for over 600 more units of housing. All of this is part of a broader effort to influence positive health outcomes through Essentia’s Healthy Hillside Initiative.
Health systems are beginning to uncover the value behind these investments not only for patients, but also for their employees. Affordable, accessible childcare, housing, and proximity to work are some of the needs being addressed by land donations.
Sanford, like many rural serving healthcare institutions, has to navigate the challenges of workforce shortages in their area and recruitment is an ongoing process. Aspirations are high for how the new home can make a bigger impact in attracting workers in Northwestern Minnesota. The Veteran’s facility that was created will help serve the broader veteran’s community by opening up space for meetings of the Veterans of Foreign Wars (VFW) and American Legion fraternal groups. The vital conditions for health and wellbeing framework emphasizes the importance of belonging and strong social support.The new Veterans Home is now part of the infrastructure supporting community health and wellness.
In our playbook we shared how a healthcare system, Dartmouth Medical, took an investment approach to a transportation project in partnership with Southwestern Community Services (SCS). In the time since, this investment has grown as Dartmouth began to see a benefit to move beyond the initial investment to playing a role in maintaining the operations. This successful partnership now runs at an annual $120,000 in support.The transportation route that was subsequently established has seen an increase in ridership and in response they have doubled their round trips since operations began. Along with other Dartmouth transportation investments they now provide free or low-cost options for riders through three regional contractors.
Filling this transportation gap benefits not only residents but also patients and employees, especially as the unaffordable housing options near the Dartmouth facility force staff to travel longer distances. Since the Dartmouth and SCS line was established, additional provided routes are accessible to link to other transportation providers opening up access to neighboring states.
Another notable area of investment for Dartmouth (a member of the Healthcare Anchor Network) is affordable and workforce housing through the establishment of a $3 million lead investment in the Upper Valley Housing Fund. Six other local businesses have co-invested alongside the healthcare system to create a $9 million housing fund that facilitates access to capital for affordable and workforce housing projects. The first of these projects were under construction in White River Junction (Population 2,766) with all the fund investors expected a 1.5% return on investment. The Upper Valley Housing Fund team was awarded the New Hampshire Businesses for Social Responsibility 2023 Partnership for Innovation Award together with Vital Communities, a local nonprofit organization that engages Upper Valley residents, organizations, and communities to create equitable solutions to challenges in the region.
In another example of its anchor role, the New Hampshire Community Loan Fund received a $3 million impact investment from Dartmouth. Together with other donors and investors that included a bank and government funding sources, this fund aims to preserve affordable housing through Resident-Owned Communities (ROC). ROCs preserve land/housing from re-development through collective ownership models. In New Hampshire, close to 9,000 people, including Dartmouth employees, now live in affordable homes managed by 145 of these ROCs. The impact investment provided by Dartmouth to New Hampshire Community Loan Fund, a Community Development Finance Institution (CDFI), enables below-market financing, technical support for purchasing, and business planning support to communities that want to become ROCs.
The Texas A&M University Colonias Program, began a partnership with the US Department of Defense (DoD) through the Innovative Readiness Training (IRT) Program in 2017. Since then, IRT has provided essential medical, dental, mental health, and veterinary services to colonia residents in five South and West Texas counties: Webb, Maverick, El Paso, Nueces, and Hidalgo. To date, the counties have received over $10 million as a direct result of IRT activities.

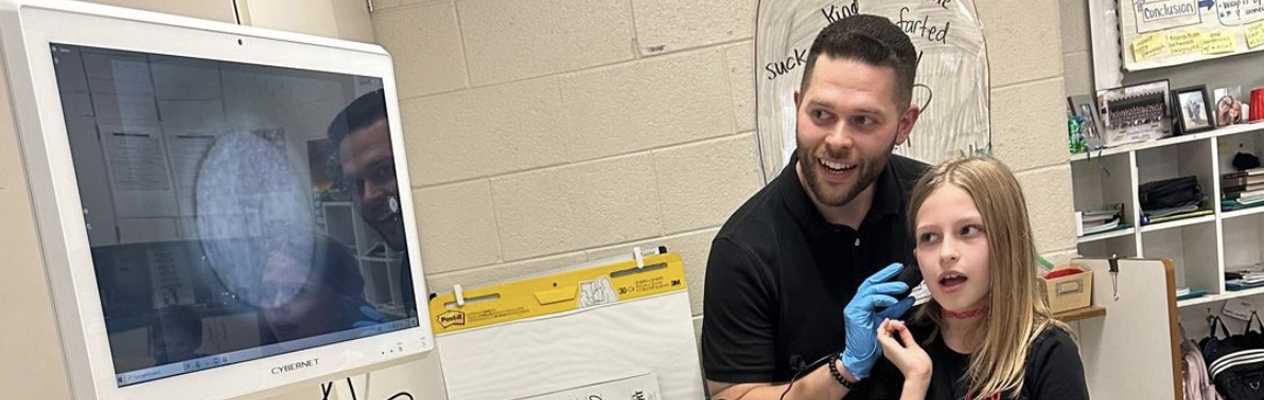
In each IRT mission delivery, the Colonias Program leads a cross-sector collaborative approach and includes the local federally qualified health clinic (FQHC) or other local service provider to provide a medical home. They have also partnered with area institutions of higher learning through either internal Texas A&M University System schools or other State institutions with 30 nursing students giving them the opportunity for hands-on learning.
A new type of IRT mission that was first introduced in Webb County, and replicated in Maverick and Nueces counties, was the use of Civil Affairs units which help gather data by going door to door and creating a Community Needs Assessment. To date, over 5,400 colonia residents have engaged with the CNA process.
The third type of IRT mission that has been facilitated by the Colonias Program includes Civil Engineering/Transportation. Colonias have traditionally been located in flood prone areas and the Colonias Civil Engineering/Transportation Program has worked to repave or level roads in these communities, helping keep these rural unincorporated areas connected to services in more populated areas.
Every branch of service can participate in IRT such that in addition to benefiting American communities, service members get real world experience with their units. IRT celebrated its 30th anniversary of providing training value through its civil military partnerships.
The main focus of the Ho-Chunk Community Development Corporation (HCCDC) continues with their innovative cross-sector approaches to supporting food sovereignty in their community.
The organization has reached many innovative milestones including the Bago Grows home gardening program, Ho-Chunk Village Farmers Market and development of the Tribe’s Food Sovereignty Strategy.
The Winnebago Food Security Task Force mentioned in the original case study is still very much in place and the coordinators of that program all work with the Farmers Market to provide food security. Executive Director Kristine Earth shared the impact a partnership with the Winnebago Wildlife and Parks Department has had in increasing the accessibility of fresh bison to families in the community with discounts available to tribe members.
Earth shared “Through our farmers market, now we’re able to touch on not only agriculture and tribal farming, but also our health care system. Offering the fresh fruits and vegetables and the Indian corn; things that will restore the health of our people.”
HCCDC is the hub for this food sovereignty initiative and is implemented alongside partners who provide programming that can range from helping residents till their own land, accessing free seeds to creation of home gardens. The opportunity to sell their own produce at the Farmers Market creates an intersection between greater food security for tribal families with the opportunity for economic mobility through microenterprises.
2024 brought another exciting update as HCCDC was awarded $2 million through Yield Giving set up by MacKenzie Scott. Earth shared how HCDC plans to lean into five key initiatives that include: housing development, commercial development, financial services, quality of life, and food sovereignty. With roughly 30% of the Tribe’s members still living in poverty, there is no doubt that this historic award will help HCCDC meet its mission.
Kentucky Highlands Investment Corporation’s (KHIC) long history of work in the state has focused on sustainable employment opportunities. As a Community Development Financial Institution (CDFI) that has served primarily small business development since 1968, they estimate that their efforts have resulted in 25,000 to 28,000 jobs created for the communities in their portfolio. In our original playbook, we described KHIC’s role in preserving local healthcare alongside First State Bank, saving a rural hospital in Pineville, KY (population 1,630) from closure as they filed for bankruptcy.

KHIC’s robust healthcare projects include two Federally Qualified Health Centers (FQHC), two rural hospitals (one of which, Pineville, was highlighted in our playbook), and three family health centers. This activity accounts for about 20% of their $100 million portfolio.
KHIC is able to sustain their service model by accessing diverse federal funding opportunities, such as the Small Business Administration (SBA), the US Health and Human Services Administration (HHS), the US Department of Agriculture (USDA), and Health Resource Services Administration (HRSA). After the CDFI’s work with Pineville, HRSA asked KHIC and Primary Care Development Corporation (PCDC) to participate in the update of HRSA’s important Health Center Facility Loan Guarantee Program (LGP), to model it after USDA’s Rural Development Business & Industry Loan Guarantee Program. Without this guarantee program, two new FQHC projects in the state would not have met the risk threshold from their lenders to make the projects viable (80% guarantee), illustrating how policy can be a critical factor that enables future multi-sector investments for health in rural communities.
Adaptive reuse, or the repurposing of space, as an option for healthcare to meet community needs and expand areas of service is becoming more and more common. Former retail spaces are often large enough to provide many services in one central location, especially useful in rural communities. Grace Health Medical Campus in Corbin, Kentucky (population 7,656) opened in Fall 2023 and is a $20.2M New Market Tax Credit Project that renovated an 84,000 sq ft former K-Mart building to provide services such as Family Practice, Internal Medicine, Pediatrics and even an innovative drive-up Pharmacy kiosk. They also have ancillary services provided by a community partner, Baptist Health Services.
This update illustrates how diverse funding sources, multiple partners, and supportive policy structures are all important factors that can help capital intensive projects that have the potential to make rural communities healthier–especially when loan guarantees are used to ensure project success and sustainabiliity.
Continuing the growth and development of the Klamath Works campus that was the focal point of the original write up, the Link Access Center has opened through a partnership by Klamath Basin Behavioral Health (KBBH) and Sky Lakes Medical Center.
The facility has served as both a collaborative behavioral health, crisis stabilization center and sobering center for the Klamath Falls community. KBBH is a Certified Community Behavioral Health Clinic Center (CCBHC), serves as the local mental health authority and works with Oregon Health Authority to manage health services in Klamath County. The Link Access Center also has several employees from the Klamath Tribes to provide culturally relevant services.
The importance of this co-locating of services on the Klamath Works campus demonstrates the commitment by the community to address issues collectively. Prior to the campus, these services were dispersed, requiring community members to make a 20 mile round trip from location to location to access housing assistance, unemployment etc. In an area with little or no public transportation this leaves vulnerabilities to individuals falling through the cracks. Additionally, the common vision to help individuals access services that meet their basic needs helps restore a sense of dignity and self-worth. Sky Lakes Medical Center also has a Peer Support Specialist from Transformations Wellness Center embedded at their office to help with referrals and care delivery.
The Klamath Works campus still attracts multisector partners delivering services addressing multiple Vital Conditions for Health and Wellbeing. Although a private non-profit, KBBH addresses their role as public health providers through the mental health lens. Amy Boivin, KBBH’s Director of Clinical Services says that they “consider mental health to be a public health mindset”, adding that they have “embraced in the last two to three years, an attitude of really prevention, networking within our community through advertising good mental health and public health messaging.”
Transformations Wellness Center is currently considering building their new facility on the Klamath Works campus since their current location is further from the community. The Klamath Works campus potential location puts them in the center of town and accessible for people who need their services.
In preparation for this update, BHPN learned that the small tight knit community is served by three different organizations that work together by providing referrals for the different services each offers. Of utmost importance will be the handing off and introduction of leadership as each organization has staff changes, including Sky Lakes Medical Center’s new CEO.
Building on Saint Alphonsus Health System belief that “housing is healthcare” the hospital continues to be, alongside their partner, LEAP Housing, great examples of creating and preserving affordable housing for their communities.
In our original case study Saint Alphonsus partnered with LEAP Housing to create Idaho’s first land trust, LEAP Housing Trust. Since the publication of the Rural Playbook, the Trust’s first development ,e Caritas Commons now consists of 14 single family homes, and two of the units have been turned over. In one instance, the previous homeowner was able to take their equity with them and the home itself was re-sold at a price point that was even more affordable than the original sale.
LEAP Housing was able to partner with the City of Boise to provide intense technical assistance to ensure that first time home buyers and those seeking housing could buy down their rate to ensure affordability. Like many in the area of affordable housing that have had to navigate the realities of increased development and construction costs during the pandemic. The homes originally sold for nearly $300,000 which was higher than anticipated, but still attainable.
The land trust model continues to spread in the state. One such community that is looking to adopt the model is Payette, Idaho, a BUILD Health Challenge 4.0 awardee, one of 13 communities across the US. This multi sector collaborative, PCHAT (Payette County Health Action Team) is composed of Western Idaho Community Action Partnership-Payette County, Saint Alphonsus Health System, Southwest District Health, Western Idaho Community Health Collaborative, St. Luke’s Health System, and Blue Cross of Idaho Foundation for Health. PCHAT is a rural Idaho community collaborative engaging residents to address housing needs using collective impact to streamline and improve preventative services in order to address social influencers of health. This model has proved to be of great interest to this small rural community because of the challenge around providing single family homes in a market where the market rate of $500,000 was unattainable for too many residents.
The creation of multifamily communities in rural communities around the state is still met with some hesitation, although St. Alphonsus continues to work on community education and outreach, seeking to destigmatize these types of developments. Given this context, the purchasing availability of single family homes versus the multifamily developments, makes the community land trust model a great entry point for smaller rural communities to experience these innovative housing solutions.
The Tippah County Hospital in Ripley, Mississippi featured in our original rural playbook opened in May 2022. In a State where Medicaid has not been expanded, this new 56,000 square foot facility with 25 beds and the addition of surgery to its medical services, is enhancing primary care in a rural county where nearly 16% of the residents live below the poverty line . The hospital received the distinction of being a 2020 Non-Metro Qualified Low Income Community Investment (QLICI) of the Year Award Recipient, and the project is a great example of home-grown success, with all the investors based in Mississippi. The investment is well made and has already had significant economic impact on the community, explained Tippah County Hospital CEO, Dr. Patrick Chapman, both directly with the hospital’s 165 staff drawing salaries totaling $18 million and indirectly creating an additional 322 jobs.
One of the partners in the original project, HOPE is a family of development organizations dedicated to strengthening communities, building assets and improving lives in the Delta. It is composed of a regional credit union (Hope Credit Union), loan fund (Hope Enterprise Corporation) and policy center (Hope Policy Institute). We caught up with staff at HOPE who shared a number of programming initiatives launched by community leaders to enhance the quality of life of residents in rural areas.One such story occurred in Drew, Mississippi (population 1,737) that lost their grocery store and prospects were dim as studies indicated that the demographics and purchasing power of the community couldn’t support a brick and mortar grocery store, even as small as 2,000 square feet. The community mobilized and advocated for access to food as a development priority. HOPE was instrumental in funding feasibility studies.
Navigating the barriers to sustaining a grocery store model, the community pivoted and in partnership with local non profit, We2gether Change created an alternative solution in the form of an online delivery service called Grocery Online Ordering Delivery Service (GOODS). GOODS provided an online ordering system and through strategic adaptive reuse, an old armory was repurposed to serve as cold storage. Through purchase of a refrigerated van, groceries are sourced from the Walmart in Cleveland, Mississippi, about 16 miles away.
This community-driven solution has since been replicated in nearby Shaw, Mississippi (population 1,385) with philanthropic funding from the W.K. Kellogg Foundation and both programs cooperate to share the refrigerated van, as a way to approach sustainability and management of costs. The community organizing successfully alerted philanthropy that the market had failed to meet the community’s needs that were ultimately met through local leadership combined with multi-sector partnerships for a locally tailored solution.
Featured in the original playbook, the ProMedica Adrian Ebeid Neighborhood Promise in the eastern corridor of Adrian, Michigan was created through multisector partnership and has continued to strengthen a community-driven approach to addressing the social determinants of health for a population of approximately 11,000, where about 30% of the population live at or below the poverty level.

Staffing the ProMedica & Adrian Ebeid Neighborhood Promise place-based investment has now yielded a team of four who are working diligently to foster and build trust in the community that they work with. This team realized that their strategic plan for services had to adapt to the needs of the community, and not the other way around.
Two overarching themes surfaced in the playbook were building trust and social capital as well as the process of reflecting on system biases where systems may exclude portions of our community.The Ebeid Neighborhood Promise staff launched community planning sessions In Summer of 2022, focusing on topics including health, jobs and financing, housing, and education. The goal of the sessions was to ensure they were reaching what the community wants or values the most. They felt they needed additional ways to engage with the community to gather community input and decided to invest in community engagement efforts. Through this pre-implementation phase they used this feedback to set strategies and priority areas for their work ahead.
They now offer services, available in both English and Spanish, co-located in an Adrian Public School that has opened its doors to programming. The staff are also able to work out of this community-based location that also provides an expanded level of support to the community. The school location has facilitated meeting the community in a space that they are familiar with and is available during hours not traditionally held by service providers. This space is popular with other service providers who often may have program and service focused funding but lack a community space to hold programming.
These services are based on the priorities that the community has emphasized. Community priorities shaped the development of these services as ProMedica Adrian Ebeid Neighborhood Promise realized one of the barriers to participation in programming was a lack of childcare. Their Parent Network Series and Getting Ahead (Bridges Out of Poverty) programming presented by partner organizations help make these programs accessible by providing childcare and free healthy dinners.
One lesson that was shared loud and clear by the community was that the ongoing trust must be earned and fostered. With documented mistreatment from the healthcare sector of marginalized communities a reality, learning to navigate to processes of healing becomes of central importance. Acknowledgment is the first step to reconciliation and growth. ProMedica approaches their work with the community not from a position that proclaims to have solutions, but from a willingness to work hand in hand with the community to identify areas of opportunity. This work requires a balanced approach to programming that prioritizes community needs rather than checking boxes on grant deliverables.
The ProMedica team is happy to also “show up to anything that they are invited to” nurturing new relationships and seizing opportunities to gauge interest from other groups within their communities. This unrestricted approach to their relationship building has produced new and early wins. For example, engagement with the Latino community in the area was helped by their introduction to two Latino Catholic congregations. Because ProMedica was endorsed by the trusted community leaders of these congregations, the ProMedica Adrian Ebeid Neighborhood Promise team was invited to share resources and events for the creation of a shared understanding to address quality of life advancements.
Wagner Community Memorial Hospital (WCMH) continues to serve the greater Wagner area in South Dakota with close to one hundred staff through innovative partnerships as an anchor institution in the community. The 1,500 residents of Wagner are part of a larger 3,500 person service area for the hospital. In following up on the major retailer that was brought in to the community that was mentioned in the original playbook, the sales tax rebates ended and that retailer closed due to its parent company declaring bankruptcy. However, the project demonstrated the feasibility and another larger national retailer has been doing quite well serving the community in that space.
Since the playbook WCMH has been in dialogue with partner Wagner Area Growth, a non profit community economic development agency, to address two pressing community issues that often have great impact on rural healthcare institutions: childcare and housing.
An innovative solution is emerging with WCMH leading the creation of a $250,000 loan fund to address these two challenges. The loan fund will provide a 0% interest loan with a 10 year amortization and 5 year term with payments not due until the borrower has sufficient 30 day funds. WCMH is leading with a $125,000 investment and planning on serving as the managing partner for this loan fund with the remaining 50% coming from community businesses and investors.
WCMH already has three additional investors for $120,000. A local nonprofit daycare that will use the funds to purchase and renovate a larger space. Aside from addressing an identified community need by increasing capacity of serving 30 to 60 children, this investment will also have an economic impact as they will grow their staff from 5 to 12 full time employees while potentially increasing or retaining the workforce by 30 . Because of a new management agreement with Rural Office of Community Services (ROCS), a private nonprofit agency serving the residents of South-Central & South-Eastern South Dakota, the daycare staff will receive significant wage increase to a new minimum of at least $15 per hour, and access to healthcare benefits.
WCMH hospital staff have an average age of 35, and with it the demand for childcare continues to grow, recruitment and retention are key challenges for rural healthcare and WCMH with loss of just one RN estimated to cost around $75,000 to replace.
In addition to childcare needs, Wagner Area Growth is interested in creating attainable housing for the community and is in discussions for potential housing investments alongside with the local school district who have funding for housing teachers.
Palmetto Care Connections (PCC) work connecting eligible healthcare providers to broadband infrastructure was featured in the original playbook. Through cross sector partnership with South Carolina Telehealth Alliance (SCTA), they have helped South Carolina residents gain greater access to health services both before and during the pandemic with this work being recognized in February 2023 receiving the Redefining American Healthcare Award by the Healthcare Leadership Council.
Since receiving the award, PCC has continued to educate and expand the broadband consortium where they help eligible healthcare providers to receive subsidies from one of the Federal Communications Commissions (FCC) programs, Healthcare Connect Fund Program (HCF). HCF provides up to a 65% discount on eligible broadband connectivity expenses for eligible rural health care providers including rural health clinics, federally qualified health centers (FQHCs), public health departments or large healthcare systems where infrastructure needs constant updating for care delivery.
PCC’s digital literacy education and training introduced in the original case study continues and although originally programming started with seniors, success has led to waitlists as demand for this programming widened. Their module content includes internet safety and how to engage with a telehealth visit and has been expanded to include health literacy and how patients can be involved in their own healthcare. 95% of the participants in the digital literacy program are African American with growing interest in developing modules in Spanish further creating greater access.
When this case study was originally published, the PCCs digital literacy programming took place in person over the span of several days. They have since expanded to accommodate online training in response to the many individuals who experienced barriers in attending in person, due to distance and/or mental or physical conditions that made it challenging for their participation. It required them to come up with a unique way to “meet the patient wherever they are and wherever they could get to”, shared PCC’s CEO, Kathy Shwarting. In May 2024, they distributed the first devices to Medicaid recipients to pilot modules that, once completed, unlocked access to 12 months of cellular service. After this period, the initiative provides digital navigators to assist the recipients in accessing subsidized cellular service.
One success story involved a recipient of the program, who utilized the access to internet services to assist her in continuing her education, resulting in her pursuing an LPN nursing degree. She was able to transition out of public housing while enhancing her quality of life through meaningful work. She now works as a full-time Digital Navigator for PCC. While this is something that PCC did not set out to do originally, they have found this and other types of success stories clearly illustrate the upstream effect on multiple aspects of a patient's well being that can come from providing access to broadband services.
Preservation of existing affordable housing is an important tool in meeting the housing needs of communities. Intermountain Healthcare and Utah Housing Preservation Fund (UHPF) were the focus of a 2021 BHPN Community Close Up describing the establishment of the Fund managed by the Utah Non Profit Housing Corporation, as an avenue to preserve the state’s most affordable housing units. Since then this work has grown to a portfolio of 768 units across ten properties spanning Salt Lake, Tooele, Summit, and Washington counties in Utah.

UHPF, with its diverse funding and programming partners has since made a commitment to a goal of investing around 30% of their portfolio in rural communities in Utah. At the time of BHPN’s Community Close Up ,UHPF hoped that the Utah State Legislature would become involved in the fund and subsequently this has materialized in the form of a $52.5 million contribution to the fund, with $10 million being directed to the fund by Utah Governor through his 2023 housing plan. In 2022, Comenity Capital Bank joined American Express, WCF Insurance and other private philanthropy to help UHPF raise a further $54 million. New impact investors for 2023 include Square and Optum helping UHPF get closer to their $250 million equity goal and hopes of serving 1,000+ units by the end of 2024.
UHPF’s preservation programming has extended to other parts of the State of Utah, with their latest acquisition of Sunset Springs in St. George, located in the southern part of the state. Previously owned by a local family, selling to UHPF as opposed to a conventional buyer is estimated to have helped residents avoid potential rent hikes of up to $300 per unit. This model has been spreading to other states with UHPF receiving inquiries from the Nevada Housing Coalition and a Houston, Texas based nonprofit interested in partnering with Memorial Hermann, one of the largest not-for-profit health systems in Southeast Texas.
An interesting partnership that UHPF has entered into is with Esusu, the leading financial technology company that is leveraging on-time rent reporting to the three major credit bureaus to establish and boost credit for participating residents. Additional programming includes Esusu Rent Relief, which is an interest and penalty free loan paid directly to UHPF, creating a safety net for those that may otherwise miss a rent payment due to financial hardship. The terms are 12 months to pay back up to three months of rent with this program.
In 2023, 36 UHPF tenants established a credit score for the very first time while 69 tenants improved their credit score since enrolling. 336 tenants are increasing their scores through the on-time rent reporting. Lastly, 7% of tenants have been moved subprime to prime borrowers while tenants with established credit before enrolling have seen an average increase of 41 points to their credit score.
UHPF was recognized in 2022 with a Common Good Award from the non profit Envision Utah, and is still working on additional programming at the community level to respond and partner with Intermountain and other healthcare providers to create a positive community for their residents to enjoy.
Mackinac County is a rural community of just under 11,000 residents in Michigan’s upper peninsula. Despite a vibrant tourism industry, Mackinac County faced a common threat affecting many rural communities, hospital closure. In 2008, Mackinac Straits Health System (MSHS) forged several strategic community partnerships to save the area’s hospital. One of those partners included the county’s largest year-round employer, The Sault Ste. Marie Tribe of Chippewa Indians. By forming a collaboration rooted in trust and guided by a shared need, MSHS and the Sault Ste. Marie Tribe of Chippewa Indians turned the tide. Instead of closing the doors of another rural hospital, the partners opened a state-of-the-art healthcare facility and tribal health clinic.

This primer makes the case for multi-sector approaches that increase community-centered investments to support opportunities for all individuals to live long, healthy lives, regardless of their income, education, race or ethnic background. Acknowledging the unique opportunities and challenges to working in rural areas and small cities, we recognize the importance of incorporating resources that reflect these realities creating freedom for locally generated solutions to accelerate through innovative partnerships. The primer provides tools such as a jargon buster, partner finder, and more.

This live conversation, which aired on September 13, 2022, explored A Playbook for New Rural Healthcare Partnership Models of Investment, highlighting core strategies used by healthcare entities in rural areas leveraging multisector partnerships for health and well-being as examples for others to follow.



Our Crosswalk essay, co-published with Shelterforce Magazine, shares examples from Kansas, Vermont, Wisconsin, and Virginia, where rural hospitals are pioneering creative partnerships with community development that pave the way for further investments in their communities.

Small towns, however, face unique hurdles in economic development that require a different blueprint for community development than in urban areas. This Crosswalk essay explores several efforts to unlock investments in rural communities in order to improve overall health and well-being in rural America.
In this brief 20 minute Video Snapshot, Build Healthy Places Network’s Ruth Thomas Squance speaks with Carrie Henning-Smith, assistant professor at University of Minnesota School of Public Health and Deputy Director of the University of Minnesota Rural Health Research Center, whose work centers on health equity, with a focus on rural residents, older adults, and historically marginalized populations.
The two discuss the important contributions philanthropy brings to community development and health partnerships in rural areas. Allen Smart also provides examples of philanthropy’s key role in accelerating investments aimed at improving health and well-being in rural communities and lays out ways community developers can connect with the philanthropic sector.
This section features a collection of resources from external sites with a rural and small-town focus relevant to organizations creating cross-sector health partnerships and increasing community investment.
A guide providing communities with information on applying for a portion of the $1.2 trillion in funding now available through the Bipartisan Infrastructure Law.
Outlines a framework for how to approach rural development successfully and showcasing stories of progress in different communities—as well as highlighting recommendations for action by policymakers, practitioners, funders and researchers—the editors and authors hope to advance this important goal.
An outline of opportunities to reframe rural economic development through an asset-based lens from the Urban Institute
Focuses on opportunities to build on the unique strengths of rural places throughout the United States to uplift local solutions for economic prosperity and resilience. Developed by the Rural Development Innovation Group of the Aspen Institute.
